Tissue Viability Team
On this page
- Download leaflet
- What is a pressure ulcer?
- Implications of having a pressure ulcer:
- Ways to prevent a pressure ulcer:
- Your Healthcare Professional / Carer will:
- Equipment that can help prevent pressure ulcers:
- This leaflet has been produced to support you / your child in making informed choices about your care
Download leaflet
Helping to Prevent Pressure Ulcers (2MB vnd.openxmlformats-officedocument.wordprocessingml.document)
What is a pressure ulcer?
A pressure ulcer is an area of damaged skin caused by pressure that may be known as ‘bedsores’.
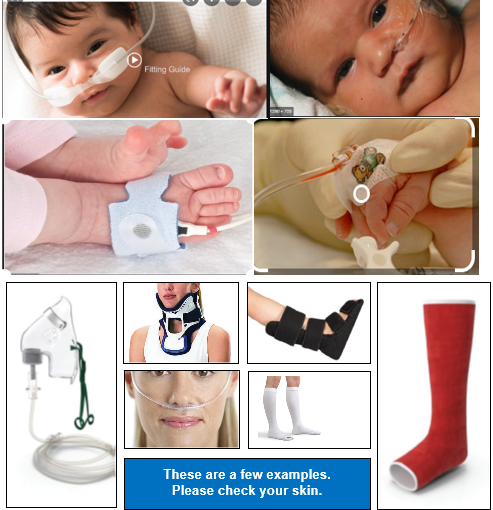
Pressure ulcers can happen by sitting or lying in one position for too long without moving. Or from any medical devices you / your child may be using. There are a few examples below.
If there is pressure to an area, blood cannot circulate causing a lack of oxygen and nutrition to the skin. If the pressure continues, then damage can occur very quickly.
If the skin changes colour, feels hard, if a warm area develops and if there is a loss of feeling or pain in an area, this may be a sign that a pressure ulcer is developing.
If you / your child don’t move, or are unable to move, you / your child may develop changes to your skin such as a red or purple area which can become sore, patches that have become very hard, patches that are soft or boggy or patches that are darker than they may usually be.
Early signs of a pressure ulcer
Redness, discomfort, pain, patches of hard skin, blue/purple patches, blisters or visible skin damage or area’s that are cool or hot.
Report any skin changes immediately to your carer or healthcare professional who can advise on pressure area care.
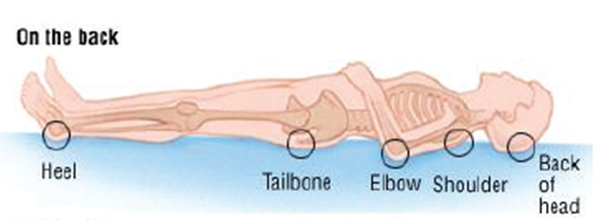
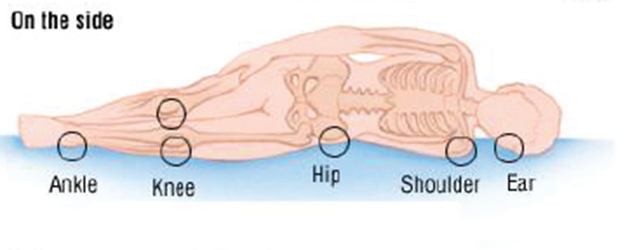
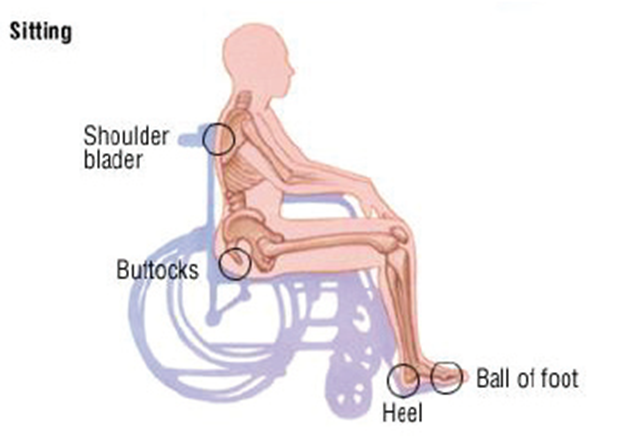
Where are pressure ulcers most likely to develop?
Usually on the parts of the body which take your weight and where the bone is close to the surface. They can take a long time to heal and are painful. Sometimes they get infected. It is much better to stop this from happening.
Some of the areas most at risk are shown below:
Be aware that some essential devices can cause pressure damage.
Implications of having a pressure ulcer:
People who have had a pressure ulcer describe them as something that;
- Was “embarrassing and smelly, got infected and stopped me doing what I wanted to do”
- made me feel like a burden, really unwell and stopped me going to school or having a social life”
- was “painful, caused broken sleep and even stopped me sleeping at all”
- Pressure ulcers can take a long time to heal and could mean you have to stay in bed for a very long time, months.
Ways to prevent a pressure ulcer:
A good way to remember this is ASSKING, this stands for;
- A risk assessment – will be completed. If you are at risk a care plan appropriate to your / your child’s needs will be made with you.
- Skin Inspection – Check your / your child’s skin as often as you can. Tell someone if you feel sore or uncomfortable, particularly if this is on your heels or bottom. If you are unable to feel if you are getting sore, try to move more often. If you have any contracted limbs it’s important that they are checked. Do not rub skin as this can remove the top layer causing damage.
- Surface – If you / your child are assessed as being at risk of developing pressure ulcers you will be offered special equipment, which is discussed below. This can help to prevent a pressure ulcer occurring. It is also very important that your chair is the right height and width for you, to prevent you sliding. This can damage your skin.
- Keep moving – This is very important. Stand or walk as much as possible, or if in bed try to roll onto alternate sides as often as you can or as discussed with your health professional. Keep moving as much as you can. If you can walk around please ensure that your footwear fits correctly to prevent skin damage. If you / your child are assessed as being at high risk of developing a pressure ulcer and choose not to keep moving, this will lead to you developing very severe damage that can put you at risk of very serious infections.
- Incontinence – it is important to deal with any continence concerns as these can damage your / your child’s skin and make you more at risk of pressure ulcers. If you develop sore or chapped skin, let your health professional or carer know. Use a barrier cream to protect skin and wash with a mild non-perfumed cleanser.
- Nutrition –plays a very important role in preventing pressure ulcers. Nutritional needs will be discussed with you and a plan made to ensure that you / your child are eating and drinking what you should.
- Give information – it is important that you understand the information given to you, if you are unclear please speak to your health care professional or carer.
Your Healthcare Professional / Carer will:
Look at your / your child’s skin in line with the plan of care agreed with you. They may need to ask if they can look at embarrassing body parts of your body i.e. your bottom. They will ask you / your child to change your position, or if you are unable to, advise carers to assist you. This will be planned with you / your child.
Advice might include:
- How to adjust your / your child’s sitting and lying position
- How often you need to move or be moved
- How to support your feet and elevate your heels
- Which equipment you should use and how to use it
Your care givers will be advised of the best way to assist you / your child to reposition if you cannot move yourself. This will be discussed at each contact.
If you only have a one off visit you will be provided with the information you need, in the form of this leaflet and a discussion about how you can help yourself / your child to prevent pressure ulcers. It would be beneficial to share this leaflet with your family members or anyone who has any input into your care, to raise awareness of how to prevent pressure ulcers occurring.
Equipment that can help prevent pressure ulcers:
Your plan of care may include specialist equipment such as;
- A special bed – Do not use your heels to push yourself up the bed. It is advised that you lift your heels before changing the position of the bed, if you don’t it can cause skin damage.
- Special mattress – this would be filled with air or made of a special foam,
- Cushions – these would redistribute pressure while you are sitting in a chair.
- Slide sheets – these will be used to help change your position.
Your healthcare professional /carer may also use things to keep the pressure off your / your child’s heels to stop them from getting sore. This is referred to as offloading. It can be done with equipment such as specially designed boots or with pillows. These will be discussed with you / your child and you will be shown what to do with them.
This leaflet has been produced to support you / your child in making informed choices about your care
If you need any information, please contact:
Tissue Viability service
Alder Hey Children’s NHS Foundation Trust
01512824 686
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG 056