On this page
- Download the leaflet
- What is Duodenal Atresia (DA)?
- What causes DA?
- How is DA Diagnosed?
- How to treat DA?
- Treatment and care after delivery
- Are there any risks with this surgery?
- What does the operation involve for DA?
- What happens after the operation?
- How long will your baby stay in the Neonatal Unit?
- What is the outlook for your baby?
- Contact
- Other useful contacts
Download the leaflet
Duodenal Atresia PIAG 465 (264kB pdf)
What is Duodenal Atresia (DA)?
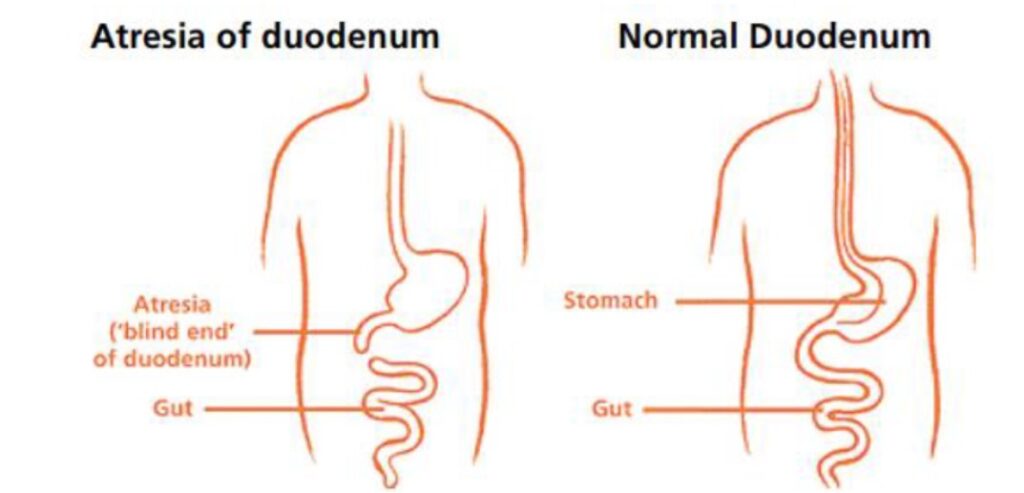
Duodenal atresia is where the first part of the bowel (Duodenum) is completely or partially blocked. This means that your baby is not able to pass the milk down into the rest of the digestive system, causing vomiting.
The condition can sometimes be diagnosed during pregnancy, around the 20 week scan or very soon after birth. Babies who have this condition require surgery in the first few days of life and following treatment, most babies experience an excellent outcome.
What causes DA?
The exact cause of Duodenal Atresia is not known and is not caused by anything you may or may not have done during pregnancy. The risk of having another baby with this condition in future pregnancies is not increased.
It is a rare condition and occurs in about one in 6000 births. It can be associated with other problems, so the doctors will examine your baby closely to check if this is the case. One third of all babies with DA have Downs Syndrome (trisomy 21). Because of this association, you will be given the opportunity to have genetic testing during your pregnancy and or after your baby is born.
Even if DA is suspected before birth, the diagnosis cannot be made until after your baby is born. This will involve your baby having further investigations.
How is DA Diagnosed?
DA can sometimes be suspected during your pregnancy on antenatal ultrasound scanning when there is large amount of amniotic fluid around your baby. This extra amount of fluid is known as polyhydramnios. On ultrasound, this swelling in the stomach and duodenum is referred as ‘double bubble’. These signs in the scan can suggest DA. Whilst polyhydramnios can be normal in many pregnancies, it can also be associated with other conditions and premature labour.
However, more detailed specific investigations are used after birth to confirm the diagnosis. A special x-ray imaging using water soluble contrast is one such investigation. During this procedure, a harmless liquid (contrast) is given to your baby, through a tube passed from his or her nose or mouth to the stomach. A continuous X-ray beam is passed through the stomach and the bowel while the contrast moves through the stomach and the small bowel. The image is then simultaneously sent to a video monitor, much like an ‘X-ray movie’. This type of imaging is most useful in identifying any obstruction or atresia.
How to treat DA?
Duodenal Atresia always requires an operation to allow your baby to feed.
Treatment and care after delivery
To begin with your baby will be nursed in an Incubator. Milk feeds if they have commenced, will be stopped due to your baby vomiting milk or a green fluid known as bile. A naso- gastric tube will be passed through his or her nose, down the oesophagus (foodpipe) into the stomach. Through this tube the stomach contents can be allowed to drain into a collecting bag attached to the end of the tube. The bag will be emptied using a syringe every 3-4hrs, thus helping to stop your baby feeling sick and being sick. It also releases any excess air from the stomach which could make your baby uncomfortable. This tube will stay in place until no longer needed. We would support the baby’s nutrition via Parenteral Nutrition (PN-special mix of nutrition given via a drip) and hydrate baby through a drip into a vein. Antibiotics will be given to reduce the possibility of any infection. Your baby should then be safe and stable and can be transferred to a surgical unit at a mutually convenient time.
Although your baby cannot take milk at this time, if you plan to feed your baby breast milk later on, (either by breast-feeding or by bottle) you should start expressing breast milk within six hours of birth. The nursing staff on the unit will be able to show you how to express and store your milk and arrange for you to have a breast pump. When your baby has recovered from the operation, he or she can then start to receive your milk.
Are there any risks with this surgery?
The surgeon will explain about the operation in more detail, discuss any worries you may have and ask you to sign a form giving consent or an e- form on line for your baby to have the operation. All the Doctors have had lots of experience in performing this operation. An anaesthetist will also visit you to explain about the anaesthetic and discuss pain relief to keep your baby comfortable after the operation.
What does the operation involve for DA?
- DA is repaired in an operation under general anaesthetic (so your baby is asleep).
- The surgeon will cut the blind end of the Duodenum and connect it to the rest of the intestine (bowel).
- This then provides a passage for fluid and food from the baby’s stomach to his or her intestine (bowel).
What happens after the operation?
Your baby will come back to the unit in the incubator to recover and you will be able to visit as soon as he or she is back. All babies are closely monitored after the operation and so your baby will be connected to monitors to check their breathing, heart rate, and oxygen levels. Your baby may or may not require additional breathing support after the operation. Pain relief will be provided with strong pain killers (analgesia) following the operation to keep your baby comfortable.
Until your baby’s intestine (bowel) recovers and starts to work, they will continue to be supported with Parenteral Nutrition. This will gradually be replaced by breast or formula milk, given through the nasogastric tube when your baby is able to tolerate this. Initially, your baby may have mouth care with your breast milk even though milk is not being given as a feed. As your baby recovers further you will be able to breast feed or feed him or her from a bottle. Over time the drips will be removed. Your baby’s wound will be meticulously observed for any sign of infection or complications.
You may feel anxious, especially while your baby is connected to drips and monitors but it will become easier in time. If you are worried about caring for your baby, please talk to the nurses who are there to support and help you. You will be able to go home or be transferred back to your local hospital once your baby is feeding properly and gaining weight. Your Health Visitor will visit you regularly. A clinic appointment will be made after discharge for the surgeon to see your baby in clinic.
How long will your baby stay in the Neonatal Unit?
The length of your baby’s stay in hospital will depend on:
- Their recovery from the operation.
- Whether they have any other medical conditions.
- Whether they were born early.
- Your baby will be discharged from the hospital when he or she is taking food by mouth without difficulty and gaining weight.
What is the outlook for your baby?
The outlook is excellent for those babies whose DA has been diagnosed and treated early and who have no additional conditions associated with it. In the minority of babies there is a small risk of future blockages occurring. The surgical team will discuss this with you and regular follow up at clinic will be arranged so that any such problems are identified and treated promptly.
Contact
If you have any concerns or worries about your baby once you are home you can call the Neonatal Surgical Unit and one of our Nurses will be happy to give you advice and reassurance.
Neonatal Unit 1C Yellow Pod
Tel:0151 252 5378
Other useful contacts
BLISS
Support for babies born premature or sick.
Website: www.bliss.org.uk
Tel: 020 7378 1122
Email: [email protected]
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG: 465