Fetal – Perinatal Cardiology Service
On this page
Download the leaflet
Fetal Tachycardia and Supraventricular Tachycardia (SVT) (242kB pdf)
Introduction
The diagram below will help to explain about Tachycardia and Supraventricular Tachycardia (known as ‘SVT’)..
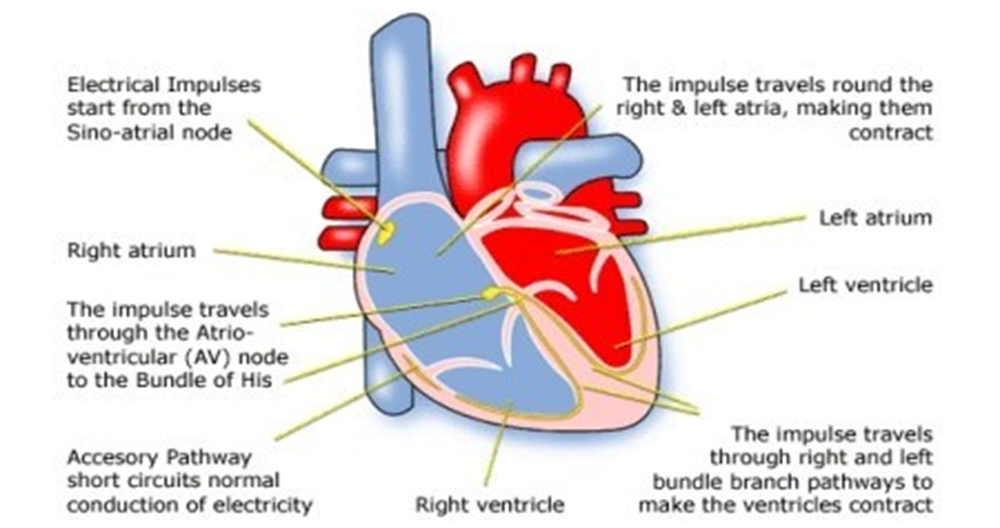
Heart Diagram with Circuit
(Supraventricular Tachycardia)
What is Tachycardia and Supraventricular Tachycardia (SVT)
A normal fetal heart rate is usually between 120 and 180 heart beats per minute. The top chambers of the heart (atrium) start the electrical impulse that travels to the bottom heart chambers (ventricles).
A tachycardia is a fast heart rate and SVT is an abnormally fast heart rate from the top collecting chambers, usually more than 250 beats per minute in a fetus.
Most patients with fetal SVT have a normal heart structure, though SVT can happen alongside structural heart disease. This will be checked at the visit to the fetal cardiologist, by doing a fetal echocardiograph (an ‘echo’ is an ultrasound scan). Most SVT occurs as an isolated problem and is due to immaturity in the conduction system, it is not usually caused by any inherited or genetic conditions.
In most cases, a fetus can cope with faster heart rates for long periods of time without too many problems. However, having a fast heart rate for many weeks, can cause the heart to show signs of failure. During fetal life this is diagnosed as ‘hydrops’ and is a build-up of fluid around the baby.
Medication and on-going monitoring of both Mum and Fetus
Where there is persistent fetal SVT, there is need to give Mum medication that crosses the placenta to slow the fetal heart rate and treat baby.
The medications used are frequently used for adult SVT, but larger than usual doses will be given to Mum so that enough of the drug crosses the placenta. The treatment we use can make Mums feel tired and nauseous, and we will need to obtain regular blood tests to check the drug levels.
If you feel very unwell following the start of this medication, you should discuss this with your fetal cardiologist.
An ECG is a test performed to look at the electrical activity of Mums heart, and you will require this test before starting medications, and regularly following this. We will give a plan to your local team to still see you regularly. We will ask that you attend for frequent reviews at the fetal medicine unit to check heart rate, heart function and check for hydrops and assess baby’s well-being. Should you have any concerns, reduced movements, or feel unwell, please contact your local team for advice.
It can take a few weeks to gain control of the fast heart rate, and sometimes a change in dose or medication type. Rarely is an admission to hospital required, but sometimes we need to change the way Mums get their medication from oral to intravenous drug therapy.
In some cases we are unable to stop the tachycardia completely, but are able to reduce the heart rate enough to maintain good heart function. In cases where the heart rate is difficult to control, your fetal team may advise early delivery to allow further treatment of the baby.
Very rarely, despite treatment, a small number of babies do not survive to delivery.
Depending on babys response to treatment we may ask that delivery is via planned caesarean section at Liverpool Womens Hospital or St Marys, Manchester. This is one of the reasons we need to see you frequently during pregnancy, and the final decision about delivery may only be made during the latter stages of the pregnancy. In those who respond to treatment and are in a normal rhythm for the last few weeks of pregnancy, a normal delivery may be possible at the local hospital.
After delivery
You should stop your medication, and baby will be assessed by the neo-natal team.
We will need a 12 lead ECG and the neo-natal team will liaise with Cardiology. Usually this will lead to an outpatient appointment in the first 2 months of life. Some cases of SVT settle down quickly and do not require any on-going treatment, and baby can go home and be reviewed in cardiac clinic.
Other babies will be transferred to Alder Hey for further assessment and could be discharged on daily oral medication. They will have regular appointments and blood tests to check levels and we can teach you how to check heart rates at home, using a stethoscope.
For babies born in persistent tachycardia they could be quite poorly after birth and require intensive care treatment.
Some babies may be born and be found to be in a heart rhythm called atrial flutter. The treatment for this is cardioversion (electrical shock to the heart with a defibrillator) which will often put the heart in to a normal rhythm. Long term medication isn’t usually needed.
In the majority of cases (9/10) this problem resolves on its own. Typically we would stop medication at 1 year of age and monitor for further signs of tachycardia. In a small percentage
(1 out of 10) children will require ongoing treatment or monitoring throughout childhood.
Occasionally episodes can stop entirely and then start again in later years, often in teenage years.
Older children will often get a clear sensation of this fast heart rate (palpitation) and be able to report their symptoms. In older children, a procedure called an ‘ablation’ can be performed to burn / freeze away the area of abnormal tissue and cure the problem.
Things to think about
Some families find it useful and reassuring to visit the units where baby is going to be. The
neo-natal unit visits can be arranged by the midwives, and a visit to the cardiac wards can be arranged with the cardiac nurse specialists.
If your baby needs ongoing admission, there is parent accommodation at both Alder Hey and Royal Manchester Children’s, called Ronald McDonald House. This is a short walk from the main hospital building. If baby is in intensive care or high dependency you can sleep here overnight or sit at babys bedside. If baby is on the cardiology ward, one parent can sleep at the bedside and one parent can sleep in McDonald House. Its free to stay there, but they will ask for a refundable deposit.
Midwife support is available at both paediatric centres. At Alder Hey, the Liverpool Community midwives have a clinic for newly delivered Mums. One of the volunteers will give you an appointment for this. Should you have any concerns about your own health, please speak to the nurse looking after baby.
Things to bring when your baby is admitted
Nappies, socks, mitts, hats and blankets.
Clothes and personal items for yourselves. We would advise indoor and outdoor clothes because McDonald House is about a 5-10 minute walk.
Feeding a baby with heart rhythm problems. Most of these babies will feed normally and we will support you with breast feeding and or expressing breast milk. We have kits and breast pumps
– discuss this with the nurse looking after baby. Some babies with persistent tachycardia may need some support with NG feeding if they are in the intensive care. If you choose to bottle feed you will be asked which formula milk you want to use.
Contacts / Further support
Children’s Heart Federation – www.childrens-heart-fed.org.uk
Heartline – www.heartline.org.uk
British Heart Foundation – www.bhf.org.uk
Children’s Heart Association (this is our local parent support group) – www.heartchild.info
Ante-Natal Results and Choices – www.arc-uk.org
Arrhythmia Alliance (for patients with arrhythmias) – www.arrhythmiaalliance.org.uk
Team contacts
Alder Hey Children’s NHS FT 0151-252-5642-voicemail checked midday Mon to Fri (excluding bank holidays)
Royal Manchester Children’s Hospital 0161-701-0664 or 0665
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG 317