Ophthalmology department
On this page
- Download the leaflet
- Introduction
- What is a cataract?
- What causes a cataract?
- What are the signs and symptoms of cataract?
- What treatement(s) are available?
- What are the side effects of my child getting or not getting the treatment?
- What are the next steps?
- What can patients with cataract do for themselves?
- Are there any implications for others?
- Does anything increase the risk of someone getting cataract?
- Who to contact for further information or support?
- Further resources:
Download the leaflet
Cataracts in babies and children (290kB pdf)
Introduction
The leaflet is aimed at providing parents, guardians and carers with information about a condition called childhood cataract. We hope that this leaflet will provide some more information about cataracts in babies and children, the treatment options, and the long term care.
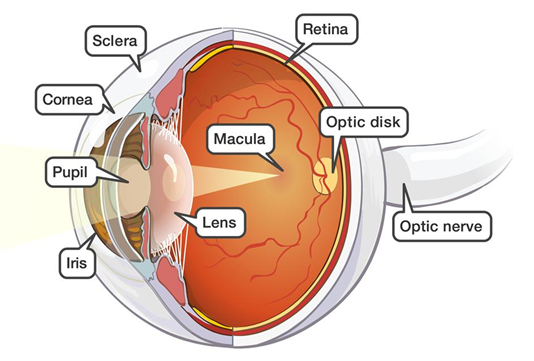
Normally light passes from the front of the eye (cornea) to the back of the eye (retina) to help us see. The cornea and the lens work to focus an image onto the retina. Information is then sent along the optic nerve to the brain so that we can interpret the image. Normally the lens is clear so that light can travel through without disruption, and it can change its shape to help improve the focus.
What is a cataract?
When the lens becomes cloudy, it is known as a cataract. This disrupts the light that enters the eye. This can result in the child seeing blurred images. Cataracts can sometimes affect one (unilateral) or both (bilateral) eyes.
Cataracts are more commonly seen in adults. However, some children may be born with cataracts (congenital), whilst others may develop them during their childhood (developmental or childhood).
What causes a cataract?
In many cases it may not be possible to identify the exact cause.
Possible causes include:
- A genetic change inherited from the child’s parents that has caused the lens to develop abnormally
- Other genetic conditions, e.g. Down’s syndrome
- Some infections picked up by the mother during pregnancy, such as Rubella and chickenpox
- Severe injury to the eye
- Certain diseases with the eye, such as uveitis
- Use of certain medications for a prolonged period of time, such as steroids
What are the signs and symptoms of cataract?
- Cataracts in babies are often picked up during the routine screening, either at birth or at about six weeks. There are no symptoms at this age that is associated with cataracts. In some cases one eye may look different to another; it may be smaller or a slightly different colour. However this can be quite subtle.
- Developmental cataracts may be associated with:
- Poor vision – bumping into things, difficulty recognising people or objects
- Wobbly eyes – rapid, uncontrolled eye movements (known as nystagmus)
- Turn in the eyes – eyes pointing in different directions (known as a squint)
- White or grey pupil – this is often seen on newer, digital cameras and mobile phones
- Glare – struggling with bright lights outdoors
What treatement(s) are available?
The treatment for your child will dependent on the severity of the cataract. At the clinic appointment your doctor will determine whether the cataract is likely to be affecting the vision and whether surgery is required.
If surgery is not required, then your child will require regular check-ups to monitor how the vision is developing. If there are signs that the vision is not developing as well as it should be, then it may be necessary for the child to wear glasses and/or contact lenses and perform patching (occlusion therapy) long term to aid vision development.
If your child requires surgery, your doctor will go through with you the process of surgery at that time. They will also provide you with a leaflet on ‘Childhood Cataract Surgery’. This details not only about the surgery, but also the essential after care in the form of glasses, contact lenses and occlusion therapy.
Despite surgery, close monitoring, use of glasses and/or contact lenses, and occlusion therapy many children are likely to have reduced vision in the affected eye(s). This is known as amblyopia. However most children are able to go to a mainstream school and live full lives.
What are the side effects of my child getting or not getting the treatment?
There are some risks associated with the surgery. These may occur within days, or could occur years after. These are described in the leaflet on ‘Childhood Cataract Surgery’.
The main risk of not having cataract surgery is the increased chance of amblyopia. This poor vision may persist even if surgery is undertaken at a later stage.
What are the next steps?
If surgery is not yet required for your child then a follow-up appointment will be made. This will be determined by the age of your child, the severity of the cataract and the level of vision. Your doctor will discuss this with you.
If surgery is required, your doctor will go through the procedure, complete the consent form and provide a date for surgery if possible. You and your child will need to attend pre-operative services when listed for surgery for an assessment.
At the time of listing for surgery, you and your child will be introduced to the orthoptists, optometrists and nurses in the department. These highly skilled healthcare professionals will monitor and assess vision development, and provide treatment for vision development as appropriate.
What can patients with cataract do for themselves?
The majority of children with cataract will be able to lead full lives and attend mainstream school. Some children may require support at school through a Qualified Teacher of Visual Impairment (QTVI) and through the Sensory Support Service provided by your local council. Your eye department will help with this process.
Children with poor vision will be refered to our Eye Clinic Liaison Officer (ECLO) who can provide advice and support. There will also be the option of being registered as sight impaired if your child has poor vision in both eyes.
Are there any implications for others?
Due to the possible risk of this being a genetic condition, we recommend that siblings are assessed for possible cataract. This includes any unborn siblings.
There is a chance that any alteration in genes that lead to cataract may be passed on to their children; therefore we recommend that any children of someone with childhood cataracts should be reviewed and monitored in the eye clinic.
Does anything increase the risk of someone getting cataract?
The commonest risk factor is a family history of cataract. The other risk factors are recurrent inflammation in the eye (uveitis) and long term use of steroid for treatment of eye or non-eye diseases.
Who to contact for further information or support?
We hope that this leaflet answers most, if not all, of your questions. If you do have any further questions please do not hesitate to contact the eye department (ext 2215) or the Ophthalmology secretaries (ext 2839, 3595) and we will do our best to answer your questions.
Further resources:
The following websites are useful for further information:
www.nhs.uk/conditions/childhood-cataracts
www.childhoodcataracts.org.uk – parental support group; has got some stories on the experiences of parents with a child with cataracts
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG 354