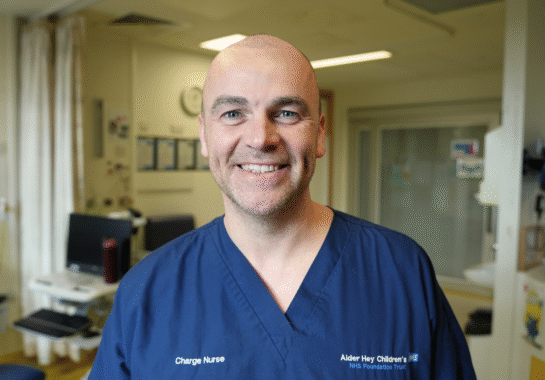
Tim Henderson is a Team Leader on the Clinical Research Facility (CRF) at Alder Hey. The CRF is our dedicated, purpose-built clinical area, where research is conducted safely and efficiently.
“As a team leader within a clinical research team, I’m often asked what clinical research actually is, why it matters so much in paediatrics, and what happens behind the scenes on a Clinical Research Facility (CRF) like the one at Alder Hey. The short answer is that clinical research is how we turn hope into evidence and evidence into better care. The longer answer is about people, partnerships, and a shared commitment to improving the lives of children and young people.
Clinical research can take shape in many forms. It includes clinical trials of new medicines or devices, studies that explore better ways of delivering care, observational research that looks at outcomes over time, and qualitative research that captures patient and family experiences. All of this work is conducted within strict ethical and regulatory frameworks to ensure participant safety, data integrity, and scientific validity.
At its core, clinical research is about learning from patients in a structured, ethical way so that future patients can benefit. Every consent form signed, every sample collected, and every data point recorded contributes to a bigger picture, one that shapes national guidelines, informs policy, and improves clinical practice.
Paediatric clinical research is not simply “adult research scaled down.” Children are physiologically, developmentally, and emotionally different from adults, and their healthcare needs must be understood in that context. Historically, many treatments used in children were based on adult data, leading to off-label prescribing and uncertainty around dosing, safety, and effectiveness.
Conducting high-quality paediatric research helps address this gap. It ensures that medicines, devices, and interventions used in children are specifically tested for their age group, developmental stage, and condition. This is particularly important for neonates, infants, and children with rare or complex diseases, where evidence is often limited.
There is also an ethical imperative. Children have the right to evidence-based care, just like adults. By investing in paediatric research, we ensure that children are not left behind in medical innovation. Importantly, paediatric research is conducted with additional safeguards, involving parents or carers in decision-making, using age-appropriate information, and prioritising the child’s wellbeing at every step.
From a leadership perspective, one of the most inspiring aspects of paediatric research is the willingness of families to contribute. Many parents choose to take part not only in the hope of helping their own child, but to help other families in the future. That generosity underpins everything we do.
Here at Alder Hey, we have a dedicated, purpose-built Clinical Research Facility (CRF), where clinical research can be safely and efficiently delivered. There are many different CRF’s across the country, all with the shared aim to bring together clinical care, research expertise, and infrastructure in one place, allowing studies to be conducted to the highest standards.

At Alder Hey, the CRF plays a vital role in supporting both commercial and non-commercial research. It provides specialist space, equipment, and staff trained in Good Clinical Practice (GCP), ensuring that studies are conducted safely, ethically, and in line with regulatory requirements. The CRF is extremely important to Alder Hey. It enables us to be at the forefront of paediatric research by providing the infrastructure needed to deliver cutting-edge studies safely within a children’s hospital setting.
The CRF is not just a physical space, it is a multidisciplinary team. Research nurses, clinical research practitioners, data managers, investigators, pharmacists, and support staff all work together to deliver complex studies. As a team leader, I see daily how collaboration and communication are essential between research teams, clinical services, sponsors, and, most importantly, patients and families.
The CRF supports a variety or research activities including Early-Phase (Phase I/II) Studies, Interventional Clinical Trials, Observational and natural History Studies, Device and Technology Studies and Academic and Investigator-Led Research. Having a dedicated facility ensures that research can be integrated into clinical care without compromising patient safety or experience.
From my perspective as a team leader, the success of the CRF and clinical research more broadly, depends on people. Leading a research team means balancing operational delivery with compassion, curiosity, and continuous learning. It involves supporting staff through complex studies, encouraging reflective practice, and maintaining high standards even under pressure.
It also means keeping the patient and family at the centre of everything we do. Research can be demanding, but it must never lose sight of why it exists. Every study visit is a child giving their time, their trust, and sometimes their bravery. That responsibility stays with us long after the paperwork is complete.
Looking ahead, clinical research is essential to the future of paediatric healthcare, and the CRF at Alder Hey is a cornerstone of that mission. By investing in research infrastructure, people, and partnerships, we are helping to ensure that children and young people receive the safest, most effective, and most innovative care possible.
As a team leader, I am incredibly proud of the work we do, not just the studies we deliver, but the culture of collaboration, integrity, and compassion that underpins them. Clinical research is not an add-on to care; it is part of care. And at Alder Hey, it is very much at the heart of what we do.”
Tim Henderson